Controlled drug delivery system endodontic paste as intracanal medication: a bench-to-chair-side case report

All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 16 May 2022
Authors
Aim: To report a new endodontic paste as intracanal medication in an immature tooth with acute periradicular abscess.
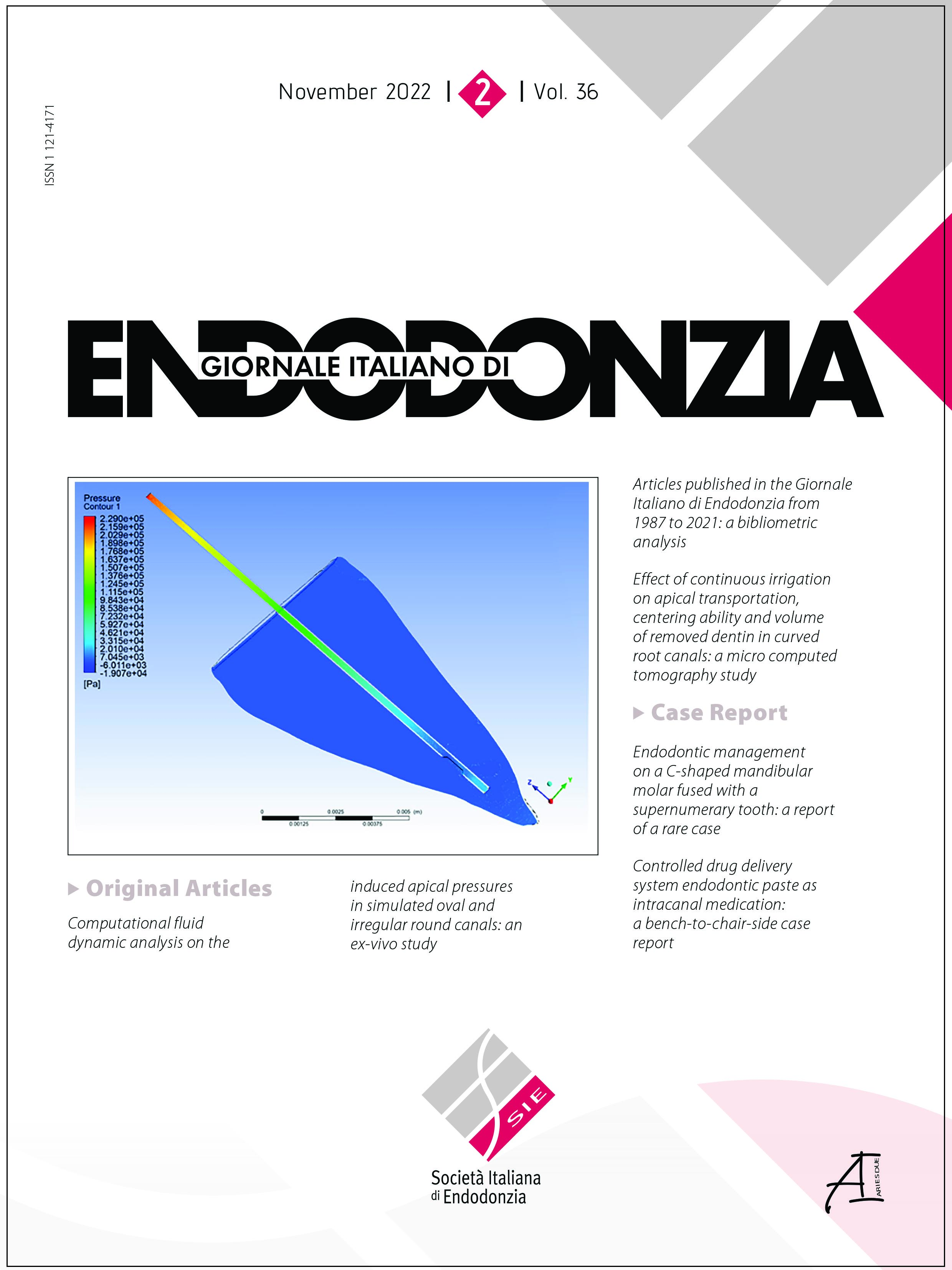
Summary: A 9-year-old male child presented to the School of Dentistry with spontaneous moderate pain and swelling in the left permanent mandibular first molar region. Radiographic and intraoral clinical exams revealed previous endodontic treatment with an extensive radiolucent area and incomplete rhizogenesis. The clinical diagnosis was acute periradicular abscess, leading to retreatment. After desobturation and chemical-mechanical preparation, the paste composed of tricalcium phosphate, calcium tungstate, amoxicillin microspheres, and indomethacin nanocapsules was inserted into the root canal system. After 5 months, there were no patient-related symptoms, and an apical barrier has formed with decreased periradicular radiolucent area was observed. The root canal filling and tooth restoration were conducted. At the 1st follow-up - 6 months later - the patient remained symptoms free, and the bone density was still increasing. At the one-year follow-up, there were no clinical symptoms, and a regression of the radiographic lesion with a zone of a hard tissue-like spicules aspect at the external tooth surface could be observed. The case's positive outcome reported a proof-of-concept of the new endodontic paste at the apexification clinical situation.
Key Learning Points
- The present case report showed promising healing results of an experimental material at a molar apexification.
- The first clinical study that evaluated an endodontic paste with controlled drug delivery systems as an intracanal medicament.
- The controlled drug delivery of amoxicillin microspheres and indomethacin nanocapsules associated with α-TCP favored the healing process and the apical barrier formation.
Supporting Agencies
Supported by grants from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – CAPES – Finance code 001.How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.